Understanding Sleep Disorders: Testing and Diagnosis
Sleep disorders can significantly impact one’s daily life, affecting everything from mood and cognition to physical health. While it’s common to experience occasional sleep issues, chronic problems require professional attention. This article delves into the intricate processes of testing and diagnosing sleep disorders, shedding light on the importance of sleep health.
Types of Sleep Disorders
Before delving into testing methods, it’s essential to understand the common types of sleep disorders:
- Insomnia: Difficulty falling or staying asleep, often resulting in daytime fatigue.
- Sleep Apnea: Characterized by pauses in breathing or shallow breaths during sleep, leading to fragmented sleep.
- Restless Legs Syndrome (RLS): An uncontrollable urge to move the legs, typically to relieve discomfort.
- Narcolepsy: A neurological disorder that affects the control of sleep and wakefulness, leading to excessive daytime sleepiness.
- Circadian Rhythm Disorders: Conditions that disrupt the natural sleep-wake cycle, such as shift work sleep disorder and jet lag.
Importance of Diagnosis
Accurate diagnosis is critical for effective management and treatment of sleep disorders. Symptoms can often overlap, leading to misdiagnosis or inadequate treatment options. Recognizing the symptoms is vital for individuals to seek the appropriate medical attention before their condition exacerbates.
Initial Consultation
The journey to diagnosis often begins with an initial consultation with a healthcare professional, often a sleep specialist. During this visit, patients are encouraged to:
- Discuss Symptoms: Detailed documentation of sleep patterns, duration, and quality is crucial. Patients may be asked about snoring, gasping for air, or daytime sleepiness.
- Medical History: Sharing a full medical history, including current medications, pre-existing health conditions, and family history of sleep disorders can provide essential context.
- Research Lifestyle Factors: Factors like caffeine or alcohol consumption, stress levels, and daily routines may influence sleep and should be discussed.
Sleep Diaries
Patients may be instructed to maintain a sleep diary for a week or two before their consultation. A sleep diary typically includes:
- Time of going to bed and waking up
- Number of waking episodes during the night
- Daytime drowsiness levels
- Use of sleep aids
- Lifestyle habits affecting sleep (exercise, diet, etc.)
This document serves as an invaluable tool, helping the specialist to better understand the patient’s sleep patterns and contributing factors.
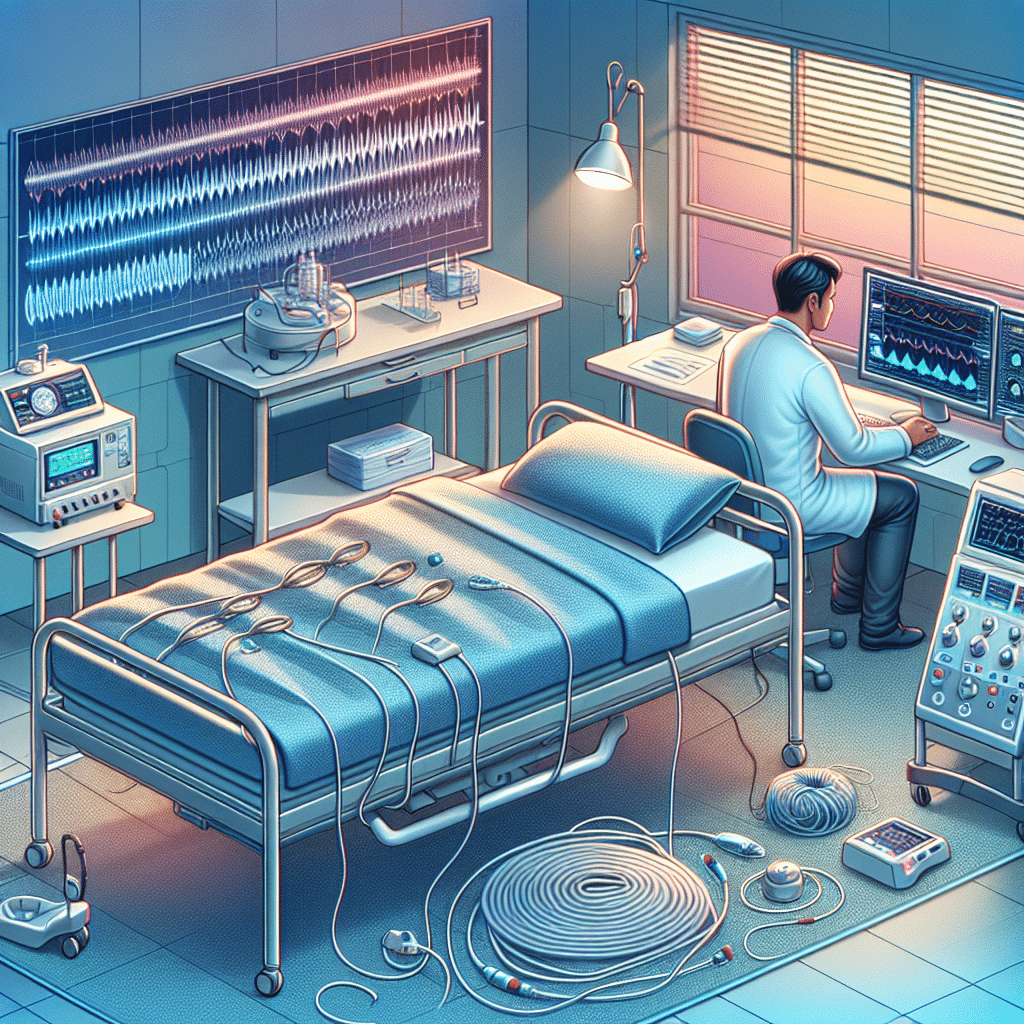
Polysomnography
Polysomnography (PSG) is a comprehensive sleep study often performed in a sleep lab. It records various bodily functions during sleep, allowing for a thorough analysis. Key components monitored include:
- Brain Waves: Electroencephalography (EEG) tracks brain activity to identify different sleep stages.
- Eye Movements: Electrooculography (EOG) records eye movements, helping to determine REM (Rapid Eye Movement) sleep.
- Muscle Activity: Electromyography (EMG) measures muscle activity, crucial for identifying conditions like RLS.
- Breathing Patterns: Sensors monitor airflow, oxygen levels, and respiratory effort, vital for diagnosing sleep apnea.
PSG can provide invaluable insights, helping clinicians identify the type and severity of a sleep disorder.
Home Sleep Apnea Testing
For suspected cases of obstructive sleep apnea (OSA), a home-based sleep apnea test (HSAT) may be preferred due to its convenience, cost-effectiveness, and increased comfort for the patient.
These tests typically measure:
- Airflow: A nasal cannula or sensor is used to monitor airflow.
- Pulse Oximetry: Measures oxygen saturation levels in the blood.
- Heart Rate: Electrocardiogram (ECG) may also be recorded to observe cardiac function during sleep.
While HSATs are less comprehensive than PSG, they can still provide crucial information and are appropriate for many cases of suspected OSA.
Actigraphy
Actigraphy involves wearing a wrist or ankle device that measures movement over an extended period, generally from several days to weeks. This method is particularly useful for evaluating sleep-wake cycles and patterns in individuals with circadian rhythm disorders or insomnia.
An actigraph measures:
- Sleep Duration: Total sleep time and awakenings.
- Sleep Efficiency: The percentage of time spent asleep compared to the time spent in bed.
Analyzing this data helps healthcare providers gauge sleep status and develop targeted treatment plans.
The Role of Questionnaires
Sleep specialists often utilize standardized questionnaires as part of the diagnostic process. These tools help assess sleep quality and daytime functional impairment. Common assessments include:
- Epworth Sleepiness Scale (ESS): Assesses excessive daytime sleepiness.
- Pittsburgh Sleep Quality Index (PSQI): Evaluates sleep quality and disturbances over the past month.
- Beck Depression Inventory (BDI): Identifies depression scales that may coincide with sleep issues.
These questionnaires facilitate a better understanding of the patient’s sleep experience and its impact on daily life.
Personalizing Treatment Plans
Once diagnosis is complete, personalized treatment plans can be developed. Based on the type and severity of the diagnosed sleep disorder, potential treatment options may include:
- Medication: Prescription sleep aids or treatments tailored to specific disorders, such as melatonin for circadian rhythm disorders.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): A structured program that helps patients change thoughts and behaviors contributing to insomnia.
- Lifestyle Changes: Improving sleep hygiene through a consistent sleep schedule, reducing screen time before bed, and creating a restful environment.
- Continuous Positive Airway Pressure (CPAP): A common treatment for sleep apnea involving a CPAP machine to maintain open airways during sleep.
Follow-up and Reevaluation
Sleep disorders often require ongoing evaluation and adjustment of treatment plans. Regular follow-up appointments allow healthcare providers to monitor progress, assess the effectiveness of treatments, and make necessary adjustments.
Through routine follow-ups, patients can also discuss any new symptoms or changes in sleep patterns that may arise, ensuring timely and effective management of their condition.
Final Thoughts on Diagnosis and Testing
The journey towards diagnosing sleep disorders is multifaceted and intricate. By understanding the types of sleep disorders, engaging in proper testing methods, and utilizing effective diagnostic tools, individuals can take meaningful steps toward better sleep health. With the right combination of professional guidance, personalized treatment plans, and lifestyle improvements, better sleep can be achieved, enhancing overall health and quality of life.